What is GBS in pregnancy?
GBS stands for Group B Streptococcus, and it’s a bacterium that lives in the gastrointestinal tract, urinary tract, digestive system, and reproductive tracts.
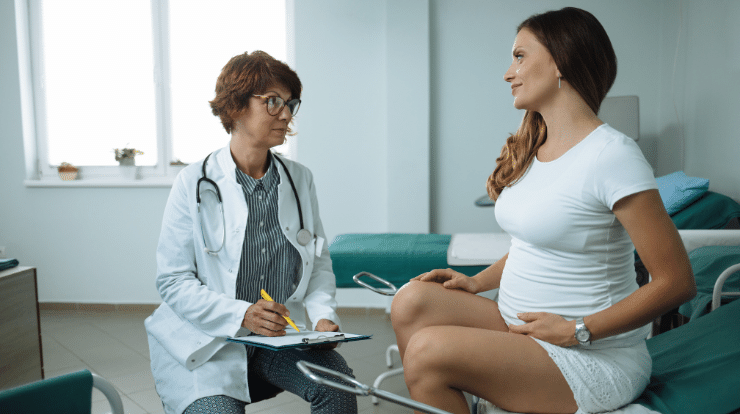
Doctors recommend that pregnant women take a GBS test and get a GBS treatment. The GBS test is typically done between weeks 35-37 of pregnancy. This is done with a swab test. If the swab test comes up positive, then the patient is treated with antibiotics. If the swab test comes up negative, then another test is done in the third trimester of pregnancy. The second test is the same swab test, but the swab is collected from a different spot in the urinary tract.
Most of the time, it’s completely harmless and doesn’t cause any symptoms. However, when a person is carrying GBS in pregnancy, it can cause severe infections in a newborn baby. Group B strep has been notorious for causing problems for pregnant moms. it’s very important to note that most babies who get infected with GBS have no signs of illness and make a full recovery.
GBS Effects on pregnancy:
Most women who have GBS in pregnancy do not experience symptoms, and ultrasound examinations show that their babies develop normally. Having GBS in pregnancy will not make your pregnancy high risk, but your chances of developing GBS in pregnancy increases your risk of:
- Sepsis
- Infection of the uterine lining
- UTI (urinary tract infection)
- Placenta infection
- amniotic fluid
GBS Effects on the baby:
When women with GBS in pregnancy have been given antibiotics, most of their babies do not get sick. But when babies become infected with the bacteria, it can develop into a life-threatening infection in some cases. Premature children are more likely to be affected by GBS as they still haven’t fully developed the immune systems to fight off all possible risks.
There are two types of GBS:
- Early-onset disease
- Late-onset disease
Early-onset disease:
can only occur in the first few days after birth. About 75 percent of those who will come down with GBS will develop it during early-onset GBS.

Symptoms of GBS in babies:
- Fever
- Drowsiness
- Feeding problems
- Sepsis (infection in the bloodstream)
- Pneumonia (infection in lungs)
- Meningitis
Late-onset disease:
Late-onset GBS, also known as Type II, tends to occur between the first week and three months of life. Type II tends to produce meningitis, an inflammation around the brain, which could cause cerebral palsy, hearing loss, or even death in some cases. However, only half of the babies with late-onset GBS have been found to have mothers who tested positive for this bacterium.
late-onset disease symptoms include:
- fever
- feeding problems
- drowsiness
How to prevent GBS in pregnancy?
If you are pregnant and at high risk of passing on the bacterium that causes GBS (group B streptococcus) to your baby, you will be offered antibiotics in labor to protect your baby. You should be offered this if you are GBS positive (you have the bacterium in your genital tract) or if you are GBS negative but you have preterm labor, long labor (over 12 hours), labor that stops and starts, or an infection (such as a urinary tract infection or pneumonia) at the time of birth.
How do you get GBS in pregnancy?
GBS bacteria has been known to be transmitted through skin-to-skin contact, for example, the contact you would have if you were shaking hands with or kissing someone who is colonized by GBS strains. Since there is also the possibility of being exposed to GBS if touching anything used by someone who carries this microbe on their body (for example, toilet seats or bath taps), sexual transmission by an infected partner could become another common vector of infection.
How to treat GBS in pregnancy?
If the test comes up positive and the fetus has been infected with the bacteria then doctors will usually recommend women receive IV antibiotics during labor in order to prevent further complications that might arise as a result of such an infection. Most commonly penicillin is used however other antibiotics may be prescribed if somebody suffers from an allergy to penicillin as many reactions are mild and temporary although it’s important to ask your doctor what side effects you should look out for.
Doctors may give the antibiotic to a pregnant woman if she has:
- Goes into premature labor, often before being tested for group B streptococcus.
- Has not been tested for Group B Strep and her water breaks 18 before her delivery date.
- Has a fever and is not tested for Group B Strep.
Effects of GBS on future pregnancies:
Holding on to your last pregnancy can lead to your next one. In a small-scale study performed in 2013, 42 percent of participants who had been diagnosed with GBS ended up having it again. This is a very important thing to keep in mind because babies cannot be vaccinated until they are born, but that doesn’t mean mothers have to go through the dreaded process of watching their infants fight for their lives after being born into this world and contracting group B strep during birth.
If you had a previous GBS infection and now another baby has developed symptoms, the best thing you can do is get those scrips ready because while you may want to hold onto your last pregnancy as tightly as possible before finally giving up that sweet little bundle of joy into someone else’s arms, it doesn’t make sense risking another poor baby fighting an infection they weren’t born with yet only to not see this one grow past infancy or take their first steps at all. But wait until labor!
If you had GBS in your previous pregnancy and the baby didn’t get it, the doctor will test you for the same in your current pregnancy. If the results come out positive, antibiotics would be administered during delivery to ensure that your baby doesn’t make a negative outcome. But if the results are negative as they should be, it is best to talk with your doctor regarding other options because we don’t want you going through that again while not really needing it.